5 Questions You Should Ask Your Patients
“And I’m sorry, but you have split ends,” he declared, pointing to my tangled tresses. “No, I don’t!” I retorted, mortified that not only did someone notice my lack of self-care but that this someone was my patient. “Yes, you do! I’m sorry, I’m a stylist. I notice these things,” he replied pointedly. I leaned back in my chair and sighed. We had gone back and forth like this for the past few months. I would start by lecturing him on the importance of medication compliance in order to successfully treat his infection and further, to avoid other opportunistic infections and ultimately death. He, on the other hand, would give me his laundry list of reasons for why he did not believe it was necessary to take his medications. His partner, a kind and serene gentleman who I will call Joe, would often play referee. Today, even Joe was speechless. I considered my options as my patient calmly gave my resident a tutorial on the ABC’s of bad hair with my mangy mop as the prime example. I could get angry and walk out. I could stay calm and stay on target and bring it back to the importance of medication compliance (again). I could tell him that I have done all I can for him and refer him to a colleague. What were my other options, really?
In his profound and thought-provoking book, “Being Mortal: Medicine and What Matters in the End,” Dr. Atul Gawande explores end-of-life discussions with patients and how physicians can approach these key conversations effectively. “We’ve been wrong about what our job is in medicine,” Gawande writes. “We think our job is to ensure health and survival. But really it is larger than that. It is to enable well-being. And well-being is about the reasons one wishes to be alive.” Gawande recommends the following five questions for those who are seriously ill, aging or frail:
- What is your understanding of where you are and of your illness?
- What are your fears or worries for the future?
- What are your goals and priorities?
- What outcomes are unacceptable to you? What are you willing to sacrifice and not?
- What would a good day look like?
At the core of Dr. Gawande’s paradigm is an unapologetic focus on what matters most to our patients: their values. Rather than wait until the last stretch of my patient’s life or waiting until he was aging or frail or seriously ill, I decided to start right away. My stylist patient felt it was unconscionable to not maintain one’s hair, just as his physician felt it was irresponsible to skip out on medications. “I’ll make a deal with you,” I said after a pregnant pause. “I promise to clean up my act with my hair if you promise to start taking your medications.” It was as simple as that. We shook on it and each month I would review his labs (marked improvement by leaps and bounds) and he would make me turn around and check my hair (slow but steady improvement). Most importantly, I got to know my patient. He had a very good understanding of his illness but did not realize exactly where he was in the course of it; a solid clarification of this put it in perspective for him. He feared losing his independence and being heavily reliant on medications. He also feared the unknown of his illness and how this would impact the job that he loved and his relationship with his partner. His goals were to flourish in his career and to stop smoking (which he did). Suffering and prolonged illness were unacceptable. A good day was spending time with his partner and styling hair without any arguments with some difficult colleagues. Today, my patient is compliant with his medications. His infection is under control and, dare I say it, so is my hair. What I am most proud of is that I have promoted the well-being of my patient, placing his values at the forefront of our agenda during each and every visit; the reasons as Dr. Gawande so eloquently puts it, he wishes to be alive.
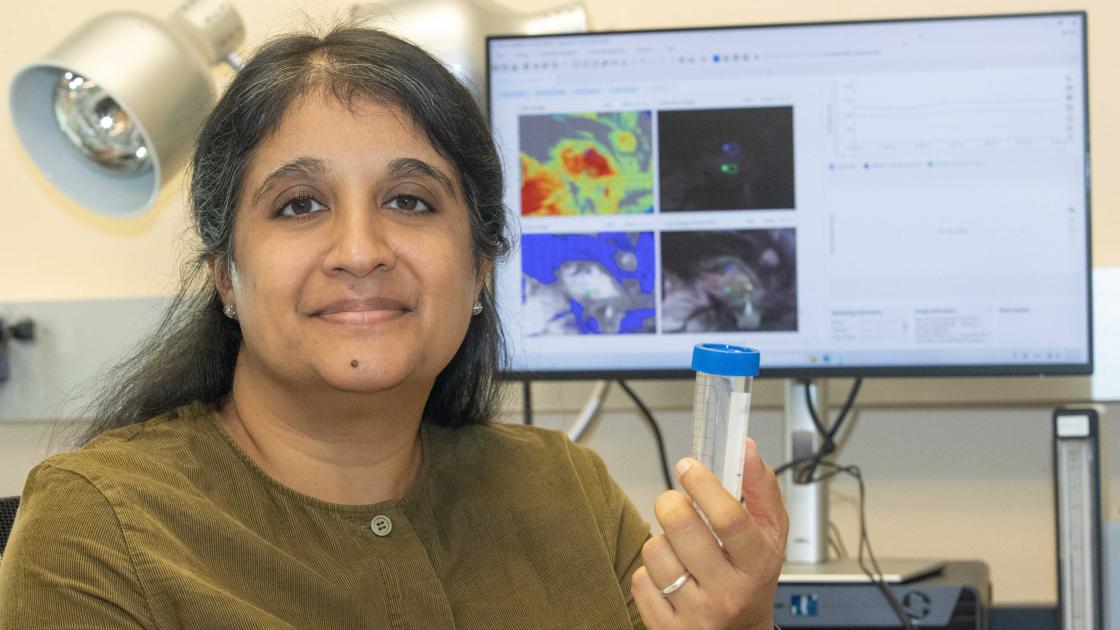
Written by Vidhya Prakash, MD, FACP. Dr. Prakash is the associate program director of the Internal Medicine Residency Program and an associate professor of internal medicine, specializing in the treatment of infectious diseases. She is also the director of SIU Medicine's Alliance for Women in Medicine and Science.