Advancements in Microsurgery over the years at SIU
A CUT ABOVE
Learning From the Best in Microsurgery
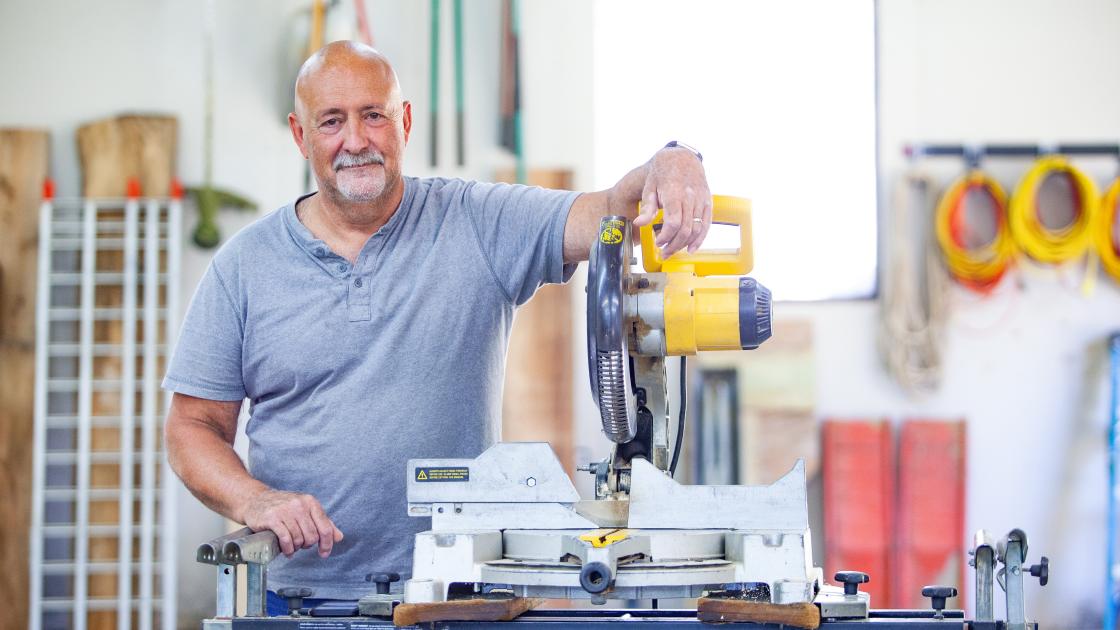
Imagine being a resident physician – doing your normal rounds in the emergency department – when you encounter a woman walking in with no pants and covered in blood. Maybe your first thought is that she has suffered some sort of trauma, until you learn that it’s her husband who suffered an accident. In the moment of crisis, she gave the only item of clothing she could, to make a tourniquet and try to prevent her husband’s loss of blood – her pants.
The only person who offered her a clean pair of pants, after she had spent several hours in two different hospitals, happened to be the surgeon who would save the use of her husband’s hand.
“It was like an old-time western movie,” said Jim Stephens, who was 38 at the time of the accident in 1997. “Michael Neumeister walked into the room and everyone snapped to attention.”
Stephens and his wife Shelly were building their first log home together, when he accidentally cut his left hand with the miter saw – leaving it attached by a small piece of skin. When they arrived in Springfield, Dr. Neumeister gave Stephens a choice: We can try to put the hand back on and see how it goes or we can simply cut it off.
“I told him, ‘Put it back on. What have I got to lose?’” Stephens said. “He asked me some other questions, and then he said as he was leaving the room for someone to please get my wife some pants and a clean shirt.”
ADVANCES IN MICROSURGERY
Microsurgery is a key component to the SIU School of Medicine plastic surgery residency program. It involves using a microscope to complete very detailed work. In the late 1990s when Stephens nearly amputated his hand, the SIU Medicine plastic surgery team was doing microsurgery, but the operations took much longer.
“Since then, technology has advanced through improved clarity and magnification on the microscopes, as well as some key tools have been developed to help us perform tiny sutures faster,” said Michael Neumeister, MD, now chair of the Department of Surgery at SIU Medicine. In 1997, Dr. Neumeister was a young surgeon, and had recently completed a fellowship at Harvard. Dr. Neumeister built his career specializing in putting limbs back together.
pecializing in putting limbs back together. “One of the reasons I wanted to work at SIU School of Medicine originally is because we did those types of surgeries,” he said. “Not all institutions were doing these, and some still do not, because it requires a certain level of expertise within a team setting, that is willing to do these long operations. They also frequently rearrange an entire day of scheduled surgeries if an emergent case presents in the ER.”
If you were a medical student in the operating room in 1997, you would see two surgeons looking in the microscope and know they are working on something, but no one else in the room would know where those surgeons were in the procedure. Now, we have large monitors so everyone in the room can see what you’re doing. That helps the general flow of the procedure, as our medical students and residents can visually be part of the entire surgery,” Dr. Neumeister said.
Medical students and residents perfect the skill of suturing, or anastomosis, in the microsurgery lab. The learners build their skills by sewing sutures on computerized veins and arteries that can track against national benchmarks; for example, if the suture is in the appropriate position, free of leaks after the repair, and if the surgeon’s hands tremored during the procedure.
“We really define the precision at which they are performing anastomosis, which builds confidence for when they are entering the operating room for the first time with a real patient,” said Dr. Neumeister.
MOVEMENT IMMEDIATELY AFTER SURGERY
Not only have surgical techniques improved over time, but post-surgical therapy has as well. SIU Medicine has an entire Hand Therapy Center dedicated to helping those with hand injuries recover through physical and occupational therapy treatments.
“We now know that early motion improves the outcomes of pretty much any surgery – with hand, shoulder, knees, hips – it strengthens tendons and bones if it’s done in a controlled environment,” said Dr. Neumeister. “We start early motion with all of our amputees these days. But in the ‘90s, that was not the case.”
When Stephens cut off his hand, the protocol was to remain still to allow the veins and arteries time to heal, for fear of tearing the tiny sutures holding them together. However, the day after his surgery, Jim was already trying to move his fingers.
“He was actually one of the patients that made us think, made us question our postsurgical therapy and showed us that we could try moving hands right away,” Dr. Neumeister said. “We thought it needed to be still and let it heal a bit first. But actually, he was doing the right thing, something we learned to be best practice a few years later.”