Don’t sleep on these tips for better rest
Experts caution: Sleep is not a luxury; it’s a necessity for good health. It’s no secret that the sleep debt is growing like the national debt in American adults. Studies show that our children are walking in our sleepy footsteps, and it’s causing innumerable negative consequences.
According the Centers for Disease Control and Prevention, young children should get 11-12 hours of shuteye while school-aged children should sleep at least 10 hours. Though they’re notorious for staying up late, teens should be getting 9-10 hours of continuous sleep.
But the statistics are waking people up.
As early as 2010, the American Academy of Sleep Medicine and the American Medical Associate passed a joint resolution stating insufficient sleep and sleepiness in adolescents is a public health issue. Eighty-six percent of teens aged 13-18 reported not getting the minimum recommendation of nine hours of sleep per night, according to a 2011 poll by the National Sleep Foundation. Several other studies show comparable results for younger children.
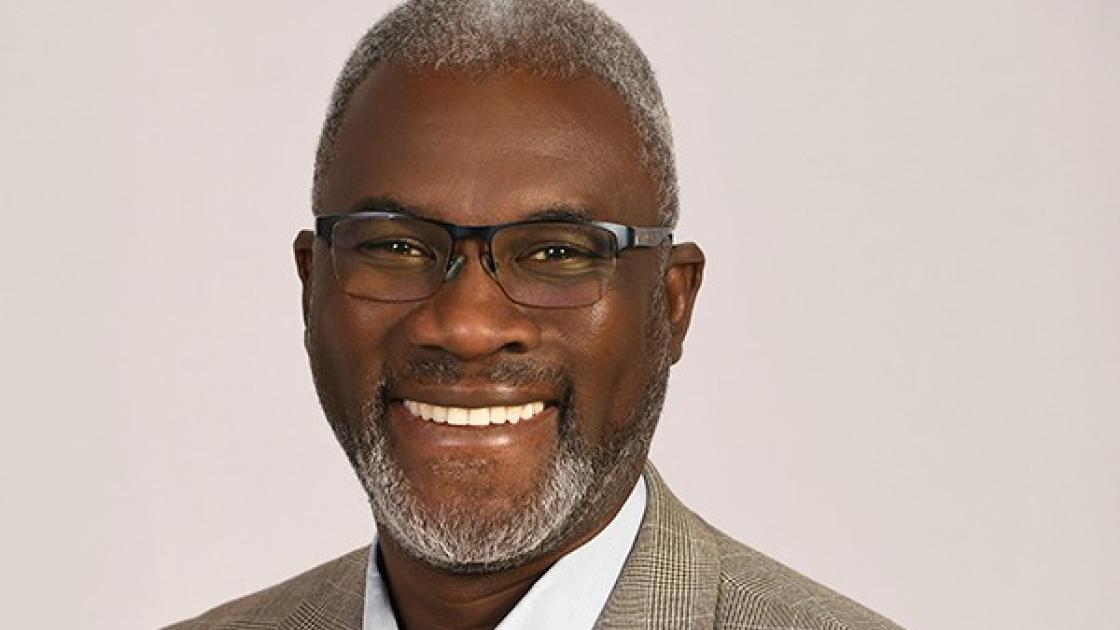
At SIU School of Medicine, Anwar Shafi, MD, assistant professor of pediatrics, is working with families in the region to help their children sleep easier and stay healthier. He is the only pediatrician in the area who is board certified in sleep medicine to evaluate and treat children with various sleep disorders and to interpret thier sleep studies. He’s on a mission to get them back to a better night’s rest.
We talked with Dr. Shafi about this important health topic:
What are some of the medical reasons children aren’t getting the recommended amount of sleep?
Physical or neurological issues can lead to nighttime disruptions that don’t allow the child a full night of rest. Sleep apnea is likely the most common issue I see. Other sleep disorders that can adversely affect children and adolescents include night terrors, sleep talking, sleep walking and periodic limb movement disorder. Some children, mainly teens, have behaviorially induced sleep deprivation.
For children who are 2 to 8 years old, sleep apnea is usually caused by restricted airflow due to enlarged adenoids and tonsils. A visit to the ENT for a tonsillectomy or adenoidectomy usually does the trick. Adolescents with sleep apnea may need the help of a CPAP machine. Sometimes children who have had their tonsils and adnoids removed in the past continue to have slleep apnea, and they may also need a CPAP machine.
Does environment or behavior play a role in sleep?
Definitely. Today’s children and adolescents are growing up in a world where stimulation doesn’t stop once the sun goes down. Activities like sports or band often take over the evenings, delaying homework time and pushing back bedtime.
For adolescents especially, the most common culprit of stimulation is the screen. In fact, most sources cite that today’s youth spend 5-7 hours a day of screen time outside of educational purposes. This includes watching TV, using computers and other electronic devices and playing video games.
Electronic devices actually have detrimental effects on sleep in two ways. First, your mind is actively engaged in what you’re doing, like checking email or playing a game. It’s hard to mentally wind down from those things. Second, these screens emit light, which alters the circadian rhythm that is responsible for helping us sleep.
Melatonin is a hormone excreted by the brain a couple hours before bedtime begins. As daylight fades, melatonin secretion is triggered. Light from the electronic devices suppresses the melatonin, making it harder to fall, and possibly, stay asleep.
Is taking melatonin supplements safe for kids?
Melatonin can be safe for children, but it’s important to realize that it helps initiate sleep. It doesn’t help you stay asleep.