Triple Aim Architect Visits SIU Medicine
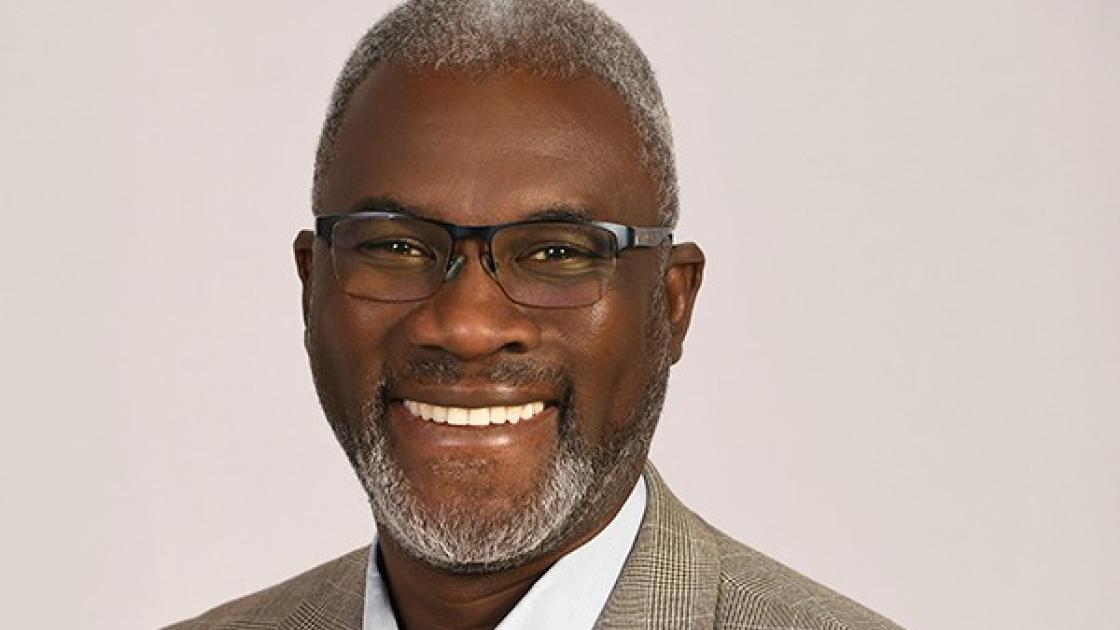
written by Karen Carlson | photographed by Jason Johnson
“It’s not about health care. It’s about the health of the population. That’s the most important thing.” So said John Whittington, MD, senior fellow at the Institute for Healthcare Improvement (IHI) in Cambridge, Mass. Dr. Whittington has more than 30 years’ experience in medicine, population health and patient safety and was one of the co-authors of the Triple Aim framework published in 2007. The Triple Aim is “one aim with three dimensions: improving the health of populations, improving the patient experience of care and reducing the per capita cost of health care.”
A family physician living in Antioch, Ill., Dr. Whittington is working with 141 organizations throughout the world on Triple Aim principles. Last November, Dr. Whittington visited SIU Medicine as the guest speaker for an Internal Medicine Grand Rounds. He also discussed the Triple Aim with SIU Medicine leaders and the Office of Population Science and Policy.
“The Triple Aim is a movement from a purely medical model of diagnosis and treatment to a psychosocial model to think about the needs of populations,” he said. “Physicians are aligned with the experience of care, not populations. We need to equip people to think more from a society and public health basis than individual transaction basis.” The Triple Aim has become the new vision for SIU Medicine. Through Dr. Kruse’s leadership, it has been coined the Triple Aim+1: “Health care that is more effective, efficient, equitable and enjoyable.” (see page 16). Dr. Whittington’s talk echoed the principles and values heard throughout SIU Medicine.
The Triple Aim’s success, he said, relies on good strategy, a strong portfolio and a good measurement system. Dr. Whittington was impressed after hearing about some of the SIU Medicine portfolio, including the population health activities, such as the hotspotting program and education initiatives such as the new third-year curriculum and MEDPREP.
“SIU has had success with rural health and so should continue that focus to make a difference,” Dr. Whittington says. “Because of your rural nature, any contributions you make is a positive thing and can be shared with other parts of the United States.”
He closed his talk with the notion that “The Triple Aim will not be achieved until it is achieved for all.” Below are excerpts from his presentation and discussions.
Dr. Whittington ... on Health Disparities
Imagine if we built cars and 80 percent of the cars look terrific, but 20 percent don’t have wheels. The US health system has these disparities from a variety of aspects.
Start with the underserved population for improvement design and work to build their trust. With some efforts, the mean or median improves, but 10 percent of population still gets left behind.
Organizations should build a multi-stakeholder coalition and work with willing partners to align the Triple Aim with your mission and determine best practices without losing sight of the whole. For example, health providers in Shelby County in Tennessee partnered with businesses and the faith community to successfully educate people about their goal to improve end-of life-care.
Organizations must understand the value proposition for the population. How are you improving their health? How do we close the gap? Are we creating barriers? We need to see with new eyes the issues we have. For example, access: One woman went to the ER 30 times in a month. A $20 investment into a bus pass for her reduced her need to go to the ER. Another example: At Health Partners of Minneapolis there was a problem of women of color getting mammograms. Transportation was an issue. The group gave women the opportunity to get a mammogram anytime they were in the clinic for any reason. It turned out to be a solution for all, which is not always the case.
...On Per Capita Costs
Health care costs too much. Doctors are big contributors to the per capita cost, yet we seldom think about it. Working on population health by itself doesn’t make sense; the practical focus should be on per capita or it’s not sustainable. The challenge is to think through the financial models that can work in these communities over time. Policy will help but won’t solve the problem. England, for example, has good policy and still has gaps.
...On Structural Racism and Unconscious/implicit bias
Most health care providers have implicit racial/ethnic bias at the same rates as the general population. That’s why we have randomized, double-blinded controlled experiments. This bias may affect how physicians interact with patients: how we communicate, deliver treatment and manage pain. Perfect care will still have disparities. We have to modify it and organize around the concept. Strategies to reduce implicit bias include putting yourself in the other person’s shoes; increase opportunities for interracial contact; See the person as an individual; imagine the individual as the opposite of the stereotype; stereotype replacement —
recognize the response is based on stereotype and consciously adjust.