
Project Self-Sufficiency
written by Karen Carlson
Last fall, Termaine Brewer wasn’t sure she would be able to give her four kids a good Christmas.
Termaine, 24, lives in Springfield with her sister, Tammy, in Enos Park. Both single mothers, they have a full house with Termaine’s four children and Tammy’s three. The house had only two beds and no other furniture. The children needed clothes. Filling the stockings with presents and the children’s stomachs with Christmas dinner was going to be a challenge. Tammy works at Help at Home; Termaine is looking for work.
A few weeks before the holidays, Termaine was dropping the kids off at McClernand Elementary School when she learned about the Access to Care Collaborative. She met SIU community health worker Shelly Weatherholt and her life changed. The collaborative has provided transportation to doctors’ appointments, public aid appointments, the grocery store and more. “Shelly’s helped me with everything,” Termaine says. The house in Enos Park now has more beds, more furniture, more food—and the Christmas tree was loaded with presents for the household’s seven children. Termaine beamed watching them unwrap toys, hats and coats. The family enjoyed a roasted chicken dinner and the kids fell sleep under new blankets—all donated by the collaborative. “It was great,” says Termaine. “And unexpected. It came out of nowhere.”
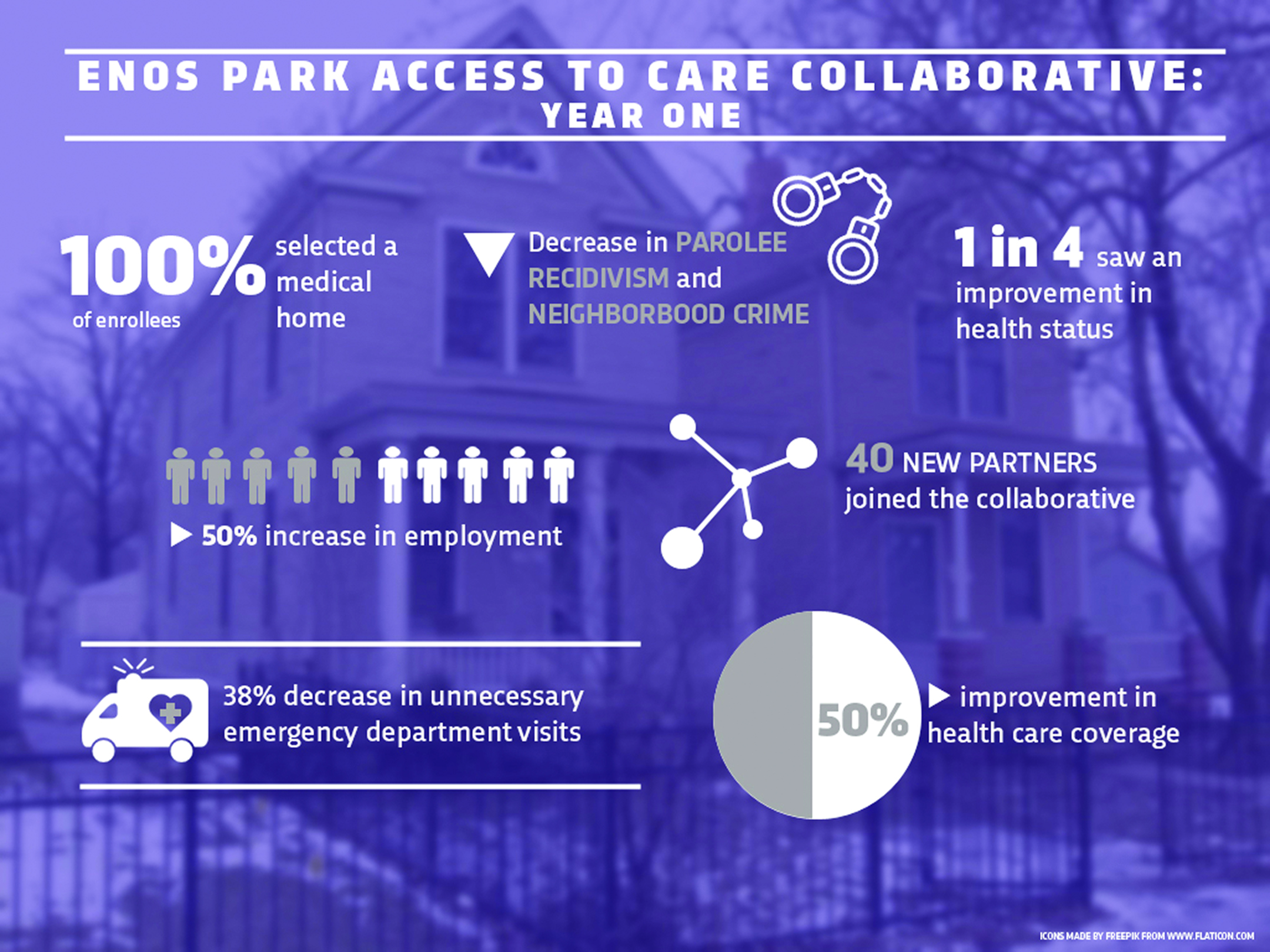
 Termaine’s story is just one of the many successes for the Access to Care Collaborative, which has helped connect more than 100 Enos Park neighborhood residents to health care, dental care, mental health care and other quality-of-life services.
Termaine’s story is just one of the many successes for the Access to Care Collaborative, which has helped connect more than 100 Enos Park neighborhood residents to health care, dental care, mental health care and other quality-of-life services.
Born out of the 2015 Sangamon County Health Needs Assessment, the health care leaders at Memorial Medical Center, HSHS St. John’s Hospital, SIU School of Medicine and the Sangamon County Department of Public Health looked for a way to help the city’s most in-need areas. The group envisioned a way to empower families in those areas to become self-sustaining, thriving members of the community.
The Enos Park neighborhood, which sits in the middle of the Mid-Illinois Medical District, was selected for the project. Enos Park has a high poverty rate, unemployment and homelessness—socioeconomic factors that contribute to poor health outcomes. The hospitals allocated $500,000 to fund the program. “Trust comes first,” says Mitch Johnson, senior vice president and chief strategy officer of Memorial Health System. “That’s where the community health workers come in.”
Those community health workers, Weatherholt and her colleague Shirley Thompson, have gained the trust of their clients and helped them obtain access to health care services. About 70 percent of the services provided were for basic needs such as housing, food and clothing. More than 400 additional Enos Park residents benefited from other services, such as a bicycle club, a summer enrichment program and holiday activities.
“The first year has been remarkably successful,” says SIU project director Tracey Smith, DNP, who facilitated the connection with SIU’s Center for Family Medicine, a federally qualified health center. “We not only met our initial goal to assist our clients to become self-sufficient for their health, but we addressed other needs, such as jobs, neighborhood safety and referrals to social service agencies.”
The program’s workers have found that helping with one issue can often lead to the discovery of other needs. For example, what started as a house cleanup for mold led to a new home for one family after a strong storm collapsed part of the roof. The team visited the family and found them sleeping in tents inside the home. The collaborative’s network of social service agencies helped move the family to better housing. “There are so many moving parts: criminal records, medicine, education. These are the social determinants of health that affect so many aspects of people’s lives,” Dr. Smith says.
“Meeting these basic human needs is vital to population health improvement,” adds Kim Luz, divisional director of community outreach, HSHS St. John’s Hospital.
But it wasn’t just medical leaders making the decisions. An advisory group of neighborhood residents collaborated with the medical professionals to help form needed programs. “We’re asking people, ‘What do you see as barriers to your health?’” Luz says. “We want to partner with them in their journey.”
With the support of the collaborative, neighborhood residents have created a surge of organized activities for Enos Park. A small group of seniors meet for the “Mature Club” to reduce isolation and loneliness; the Northside Children’s Library at Third Presbyterian Church gives youngsters a refuge after school. Dawn Mobley, originally hired as the program’s third community worker, is now a parent educator at McClernand school, strengthening the connections to the collaborative. Mobley also helps with the Summer Enrichment Program, which teaches children ages 9 to 14 life skills, career path introductions, healthy cooking and sports. Residents and the YMCA volunteered to help lead activities. “Neighborhood volunteers stabilize the program and will make it self-sustainable,” Dr. Smith notes.
The summer program was one of the two areas the community identified as its strongest need. A summer bicycle club allowed the children to enjoy group rides, led by police officers. The group rode a total of 400 miles with officers. Young bicyclists were able to safely explore their neighborhood. “This allowed the children to see police officers as ‘peace officers.’ So they know they are their friends,” Dr. Smith says.
Crime was the second area of concern for the neighborhood. Parts of Enos Park are noted for higher crime rates. Some families didn’t feel it was safe to engage with neighbors, take walks or ride bicycles. Dr. Smith and the team worked with police officers and property owners, and, indeed, officers say they’ve seen a difference in the neighborhood. Police report a 13-percent overall reduction in calls to Enos Park since the program began, and an 89-percent reduction in police calls to housing units in the area. According to officers Matt Dobbs and Chris Jones, one neighborhood residence was known for having a lot of crime activity, but “since the collaborative started, it’s gotten better.” The result is improved property investment and income for landlords. Weatherholt and Thompson helped clients obtain housing and check on them regularly to ensure they are caring for the property. “They helped fill in the gaps, such as finding the right paperwork, for people who otherwise struggle with obtaining housing, such as parolees, homeless and others,” Dr. Smith says.
One unexpected result of the collaborative’s work was the effect on parolee recidivism. The area experienced just 19 percent of parolees returning to prison, compared to the national rate of 56.7 percent.
Collaborative clients also gained access to SIU’s outreach efforts, including the medical students’ annual Day of Service and health screenings for colon cancer and diabetes. A provider alliance group learned about insurance enrollment, medical legal partnerships and Social Security enrollment. All of the collaborative clients selected a primary care medical home and enrolled in health insurance. Unnecessary emergency department visits decreased; dental appointments, primary care and mental health care appointments increased. “As hospitals continue to work toward population health management, it becomes increasingly evident that partnerships are key to improving health outcomes,” says Charles Lucore, MD, MBA, president and CEO of HSHS St. John’s Hospital.
The collaborative also is helping to grow the next generation at an impressionable point in their education. Students in medicine, social work and nursing, as well as medical residents, are gaining a new perspective on their future patients as they see clients with Weatherholt and Thompson. “The students feel empowered. It opens their eyes into asking why. Why is this—with this set of social determinants of health—happening? In the past, medicine didn’t focus on these things,” says Janet Albers, MD, professor and chair of the Department of Family and Community Medicine. “Now, it’s a new focus of population health. Beyond giving medication or ordering a test, physicians are learning about how to link patients with resources they need for the other 80 percent of health: housing, food and access to services. As we empower medical students with this knowledge, they will be more likely to ask patients and help them create a plan.”
The goal of the program is to move people to self-sufficiency, and the first year illustrated that this is an attainable goal. Almost half of the 111 clients “graduated” from the program but can still access the services if needed. “We’re amazed at how barriers can be overcome when we reduce isolation and provide help navigating the system,” Dr. Smith says. “If they need our services later, we can alleviate a crisis a lot faster.”
The leaders of the collaborative say the results have exceeded their expectations. “This success is a credit to the combined efforts of the SIU Center for Family Medicine, HSHS St. John’s Hospital and Memorial Medical Center,” says Ed Curtis, president and CEO of Memorial Health System.
 “The collaborative has yielded results beyond what any one of us could do by ourselves,” Johnson says. Paula Gramley, community benefit program manager for Memorial Health System, adds, “We chose a deep dive and a narrow focus to see if this will work. It’s grown faster than we ever expected. It’s opened the gates for more people to collaborate.”
“The collaborative has yielded results beyond what any one of us could do by ourselves,” Johnson says. Paula Gramley, community benefit program manager for Memorial Health System, adds, “We chose a deep dive and a narrow focus to see if this will work. It’s grown faster than we ever expected. It’s opened the gates for more people to collaborate.”
The Enos Park Neighborhood Improvement Association has been a key collaborator. “It’s been a fantastic experience,” says Michelle Ownbey, president of the association. “We are so excited about the results. It may help justify additional community health workers, not just in Enos Park, but in all of Springfield.”
Dr. Smith was also pleasantly surprised. “I read about these sorts of outcomes in the literature, but I didn’t expect this. We just wanted to get people access. To see the successes in action has been amazing.”
The goal for the second and third years of the program is to continue the collaborative’s long-term vision. Plans are under way to reach out to individuals who live in Enos Park and frequently visit local emergency departments, and give them access to preventive health services. A spinoff of the program is in development at Brandon Court in Springfield, a low-income neighborhood, with a grant from the United Way, and a program in Carbondale is hiring community health workers. “It’s mushrooming,” says Dr. Albers. “We’re seeing a synergy of community health workers and other parts of the health care system, reducing isolation and helping neighborhoods build trusting relationships.” They also will look at improving access to mental health and prenatal services.
For Termaine and her family, 2017 began with improved access to care. Termaine’s health insurance issues are straightened out and she and her children have a network of health providers at SIU Medicine. At an appointment in January, Termaine was able to see a primary care physician, a counselor and an attorney affiliated with the SIU medical-legal partnership. She hopes to go back to school and pursue a career in the medical field. Her children love school and are already thinking about going to college. “Thanks to Shelly, I don’t have to worry about my kids getting to their appointments. I’m hopeful for a better year.”
