Ataxic Accountant
KEY TERMS
nystagmus: An involuntary rhythmic oscillation of the eyes.
internuclear ophthalmoplegia (INO): With attempted gaze to one side, failure of the adducting eye to move beyond the midline, with nystagmus developing in the abducting eye. INO is due to a lesion affecting the medial longitudinal fasciculus on the same side as the adducting eye.
optic disk: The area of the retina entered by the optic nerve.
Marcus Gunn pupil: A pupil that may react to light but does not hold the reaction, or, paradoxically, may dilate slowly; the consensual reflex may be more prompt than the direct reflex. These changes can often be brought about by rapid alternate stimulation of the eyes with bright light, a technique called the "swinging flashlight test." It is also referred to as an afferent pupillary defect.
evoked potential test: A diagnostic test in which electrical potentials are recorded from the scalp and result from a change in the ongoing electrical activity of neurons in response to stimulation of a sensory organ or pathway. Specific types of evoked potentials include visual evoked potentials, brain-stem auditory evoked potentials, and somatosensory evoked potentials.
oligoclonal bands: A particular electrophoresis staining pattern for cerebrospinal fluid (CSF) in patients with multiple sclerosis and other inflammatory conditions. In patients with normal cerebrospinal fluid, there is a homogenous agar gel staining in the immunoglobulin G (IgG) region. In patients with multiple sclerosis, the IgG region is heterogeneous, with the appearance of several distinctly staining bands, called oligoclonal bands.
HISTORY AND EXAMINATION
History of the Present Illness
C.R. is a 27-year-old woman who sees her physician because of dizziness and difficulty walking.
She was well until 7 years ago, when she had an episode of numbness in her legs, poor handwriting, and a staggering gait, which resolved spontaneously over a 3-week period. She was well for the next 5 years, when she again developed some mild difficulty in walking. Again, she improved on her own over a 2-week period and did well subsequently. She now presents with a 3-week history of such severe dizziness that it has caused her to fall several times. Over these past weeks, her walking has deteriorated steadily, and she must now hold onto furniture in order to get around her home. She also complains of double vision when looking off to her right side.
Past Medical History
She has never been seriously ill before. She has two healthy children, ages 5 and 3. She works part-time as an accountant. Her family history is unremarkable.
Medications
None
Physical Examination
She appears healthy. Her general examination is normal.
Neurological Examination
Her mental status is normal. On cranial nerve testing, the right optic disc appears paler than the left. Her ocular motility is normal on left gaze. However, when she looks to the right, the right eye develops some horizontal nystagmus, and the left eye does not completely adduct. On motor examination, muscle tone is increased in the lower extremities; muscle bulk and power are normal. Right ataxia is greater than left on finger-to-nose testing as well as on heel-to-shin testing. The sensory examination shows some loss of vibratory perception and proprioception at the toes. She sways when standing with her feet together, and swaying is made worse when she closes her eyes. Her reflexes are brisk throughout, with bilateral extensor plantar responses. She has a broad base when she walks and occasionally lurches to one side or the other. She is unable to perform a tandem gait.
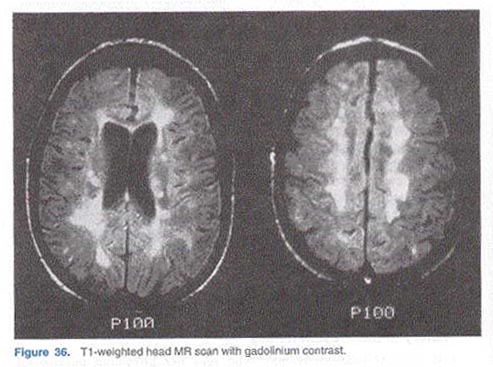
A head magnetic resonance (MR) scan is performed and is shown in Figure 36.
QUESTIONS
1. How would you characterize the course of this patient's neurological disease?
2. What eye movement abnormality is being described? Where is the lesion? On which side?
3. Why do you think her right optic disc is pale? Although not explicitly stated in the examination, what would you predict her pupillary light reaction to reveal? What is the name for this pupillary light reaction?
4. List three lesions that cause broad-based gaits. Which do you think she has?
5. Where would you localize her lesion(s)?
6. Can all her abnormal findings be explained by a single lesion?
7. What is the most likely diagnosis? Why? What is the prognosis?
8. Figure 36 reveals the patient's MR scan. What features of this head MR scan help in making the diagnosis? Why are the lesions largely confined to the white matter?
9. Besides the head MR scan, what other diagnostic tests might be helpful in establishing the diagnosis?
10. What treatments are available?
11. Both Guillain-Barre syndrome and multiple sclerosis (MS) share a similar pathologic process. What is this process, and how do these diseases differ?
