Refining a Revolution
TRAINING A ROBOTIC SURGERY GENERATION
Aspects Volume 39 No.1
Written by Lauren Murphy • Photography by Jason Johnson
It looks like something out of a science fiction film: a three-armed, six-foot tall, 1,400 pound robot with three-dimensional vision, forceps, needle drivers and cautery instruments that act as hands. Capable of performing delicate, extraordinarily precise procedures deep within the body using miniature instruments and 10 times magnification, the da Vinci ® Surgical System is the next generation of minimally invasive surgery. The robotic surgery platform is where imagination meets reality.
Robotic surgeries are becoming the norm in many specialties. Not only is SIU School of Medicine treating patients with this platform, it’s training the next generation of surgeons to use it, too.
The operating room is cool and dimly lit. The mood is light yet focused as the surgical team prepares for a four-hour, complex robotic transperitoneal partial nephrectomy (the removal of a tumor on the kidney). Three large monitors surround the patient to provide a two-dimensional view to the bedside resident, assistant and surgical technicians. A surgical nurse pushes the hulking machine to the patient’s bedside. Bradley Schwartz, DO, FACS, professor of urology, pulls the robotic arms in over the patient and locks them into place over the small area of the patient’s abdomen where Nathaly François, MD, chief surgical resident, then confidently makes three small incisions. Each incision will house an access portal, or "port," through which long, slender medical instruments connected to two of the robot’s arms can be safely guided in to the patient’s abdomen. The third robotic arm positions a stereoscopic endoscope that allows the surgeons to see in three dimensions while seated at a console a few feet away.

Left Image Caption: Known to residents as “Whoville,” these tiny, colored mountains and rubber bands help future robotic surgeons perfect their technique.
Directly below the console’s viewfinder are thumb, index and middle finger controls that enable the surgeon to transcend human physical limits by providing a greater range of motion and more precision and stability. While it is called a "robot," it’s not an independent machine – it requires the finesse of a skilled surgeon. With Dr. Schwartz’s every move, the console conveys the information to the robotic arms across the room.
And all the while Dr. François sits at an identical console, adjacent to the main console, watching her instructor’s every move in anticipation of her turn.
At hospitals throughout central and southern Illinois, the da Vinci® Surgical System is available to SIU surgeons. Springfield is home to three surgical robots, including two at Springfield Memorial Hospital and one at HSHS St. John’s Hospital. At both hospitals, SIU surgeons perform procedures in gynecology, gynecologic oncology, urology, colorectal surgery and general surgery. At Memorial, SIU School of Medicine surgeons also perform ear, nose and throat robotic surgeries.
HSHS St. John’s Hospital also acquired a dual console platform in 2009, making it the third hospital in the country to own the new system. The dual console is an invaluable training tool, says Dr. Schwartz. It allows the attending surgeon and a resident to alternate performing the surgery without the awkward transition of instruments.
Before residents can sit at the training console in the operating room, they must undergo rigorous online training. The online curriculum covers the various instruments, how to operate the robotic system and troubleshooting exercises. After the online training is complete, residents then begin working with the robot using practice instruments and the "backpack simulator."
The backpack simulator, a portable case that can be added to a robot, allows residents to develop their skillset through simulated scenarios, with or without the supervision of an attending physician. With the help of a thumb drive and the simulator’s built-in metrics, users can assess and track their skills and share their progress with prospective program directors, mentors and attending surgeons.
"By putting the robot in simulator mode, residents can go through a large number of modules – they can suture, cut, stop bleeding and more," explains Dr. Schwartz. "They practice these scenarios to sharpen their skills so that when it comes time for a real surgery, they are well prepared."
Residents can also hone their ability to suture, tie knots and improve hand-eye coordination in wet labs with a set of practice instruments that attach to the robotic arms. Training with the practice arms often involves a colorful practice environment, known to the surgeons as "Whoville." Tiny rubber bands and multi-colored, mountain-like structures, no wider than drinking straws, represent surgical targets surgeons might encounter in an actual surgery. Resident surgeons also practice their skills using an inexpensive bell pepper. "We can insert a flexible scope inside the pepper and residents can actually look around the middle of the pepper, look at the seeds, pull seeds, biopsy seeds and transfer them using the robot. In the back of the pepper, we can put in a little angiocatheter and residents can practice feeding wires and passing stents into it," says Dr. Schwartz.
Back in the operating room, Dr. Schwartz shifts control of the robot to Dr. François with the click of a button. Both heads buried in the console, the surgeons take turns cutting, clipping and cauterizing. After hours of navigating through connective tissue, fat and bowel structures, the surgeons make their way to the right kidney, where a golf ball-size tumor rests. Dr. Schwartz, who performs nearly 75 robotic procedures each year, carefully slices the tumor out of the patient’s kidney, preserving as much of the healthy kidney as possible. Dr. François reconstructs the remaining area of the kidney with slow,  precise stitches, while the bedside resident passes clips through the port to secure the stitches.
precise stitches, while the bedside resident passes clips through the port to secure the stitches.
"With the dual console, the resident is looking at everything I’m looking at; it’s exactly the same field of vision," Dr. Schwartz explains. "If I want the resident to start working, I literally just push a button and all the instruments switch over to their control." Like a driver’s education teacher, the attending surgeon can tap a foot pedal to freeze all of the instruments and pause the surgery – a helpful option when residents begin operating in their senior years of training.
Right Image Caption: The dual console, above, allows the attending physician and resident to work seamlessly through a surgery.
Dr. François says the training approach is especially helpful as a urology resident. In 2009, 80 percent of radical prostatectomies performed in the U.S. were done robotically, according to research from Cleveland Clinic. "The dual console enables the resident surgeon to see and then duplicate the teaching surgeon’s action, which helps to accelerate our learning with each experience at the console."
Training to become a robotic surgeon doesn’t come without its challenges. Dr. François, who plans to refine her skills in robotic surgery through an endourology fellowship following her residency, explains, "The biggest challenge with robotic-assisted surgery is learning how to effectively use the system, from positioning the ports to minimize collision of robotic arms, to using the foot pedals and mastering hand-eye coordination. It can take some time to get used to tactile feedback from the system without being able to feel the tissues or suture with your hands."
Upon finishing her residency and fellowship, Dr. François, a Brooklyn, N.Y., native, would like to work in a medical center with a robotics platform. "Robotics is what our patients want, so we have to be equipped to meet patient desires."
For residents who grew up in a world of texting and video gaming, learning to use the robot often comes naturally. Well-established physicians trained to perform open or laparoscopic surgeries, however, sometimes struggle to make the switch to robotics.
"It’s an ongoing effort to train older, more established surgeons in the use of robotics," says Dr. Schwartz, who is considered a renowned expert in robotic surgical training. Surgeons can find training opportunities at national meetings and conferences or by signing up for workshops and training courses. As open and laparoscopic surgeons make the transition to robotics, experienced robotic surgeons proctor physicians through their first robotic procedures. Dr. Schwartz, a proctor for the makers of the da Vinci® Surgical System, travels to hospitals to provide beginner robotic surgeons with guidance and tips to ensure the procedure goes smoothly.
Surgeons have been teasing out the robot’s best uses since 2000, when the da Vinci ® Surgical System became the first FDA-approved system for laparoscopic surgery. As more research became available, surgeons in urology, gynecology and other divisions found its benefits. Over the past decade, surgeons have determined which procedures and patients are most helped by the robotic platform.
While cardiology was once the premier specialty for using the robot, today, more than 80 percent of robotic surgeries are urological or gynecological, says Dr. Schwartz. Despite the prominent use of the robotic platform in the fields of urology and OB-GYN, Erica Nelson, MD, division chief of general obstetrics and gynecology, explains that not all OB-GYN residents will need to be trained in robotics. "For residents who know they want to primarily focus on other aspects of the field, such as women’s health or obstetrics, their time is better spent developing specialty skills related to their future practice."
 After eight years of performing open and laparoscopic procedures at the School of Medicine, Dr. Nelson underwent specialized training in robotic surgery in 2006 to become the first OB-GYN at SIU School of Medicine and in Springfield to perform robotic surgery. For Dr. Nelson, the transition came naturally. Today, she performs about a third of her surgeries robotically, depending on the complexity of the case.
After eight years of performing open and laparoscopic procedures at the School of Medicine, Dr. Nelson underwent specialized training in robotic surgery in 2006 to become the first OB-GYN at SIU School of Medicine and in Springfield to perform robotic surgery. For Dr. Nelson, the transition came naturally. Today, she performs about a third of her surgeries robotically, depending on the complexity of the case.
"The more difficult cases call for using the robot. It’s more beneficial to use the robot on patients with large uteruses or severe endometriosis," Dr. Nelson explains. "The added mobility of the camera and tools makes the robotic surgery easier than straight-stick laparoscopy."
Otolaryngologist Arun Sharma, MD, also sees the benefit of using the robot when dealing with difficult cases of head and neck cancers. According to Dr. Sharma, transoral robotic surgery (TORS), a procedure performed through the mouth, can more effectively treat tumors found within the larynx and pharynx than traditional transoral surgery through the mouth or open surgery through an incision in the neck.
"The robotic system allows the surgeon to reach parts of the head and neck that we wouldn’t be able to reach through traditional transoral surgery," Dr. Sharma explains. Prior to TORS, surgeons treated cancers within the pharynx with large open surgeries that often required jaw splints or tracheotomies and led to significant blood loss. Thanks to TORS, chemotherapy and radiation can either be avoided, de-escalated or more targeted, says Dr. Sharma. His research also suggests that patients who unde rgo TORS and avoid chemotherapy and radiation are able to swallow sooner after finishing treatment.
rgo TORS and avoid chemotherapy and radiation are able to swallow sooner after finishing treatment.
While the benefits of robotic surgery to patients abound – less blood loss, the potential for a faster recovery and the need for fewer pain medications – the robot isn’t always the best choice. "For urology and gynecological oncology, the proof of benefit is there – patients leave with better outcomes and it’s smart from an economic standpoint. But for benign gynecology and other procedures, we’re still teasing out the best uses for the robot," explains Dr. Nelson.
Though robotic surgery may be becoming the industry standard in many specialties, it doesn’t negate the need to train in traditional surgical skills, says Dr. Schwartz. "I feel very strongly about training residents in laparoscopic skills. If they go to a rural community that doesn’t have a robot, they can’t compete with anybody." The professor of urology balances performing surgeries laparoscopically and robotically, depending on the complexity of the surgery, the wants of the patients and the needs of the residents. "At the bedside of a robotic surgery, residents can learn and get used to passing instruments, suctioning and using clips – the same things they would do in a laparoscopic surgery," says Dr. Schwartz.
Dr. Nelson agrees. "You can do robotics without being good at conventional laparoscopic surgery, but you’re going to be a better robotic surgeon if you have skills as a laparoscopic surgeon." According to Dr. Nelson, about three-fourths of OB-GYN residents choose to pursue robotic surgery training.
Ten years ago, Dr. Schwartz predicted the robotic surgical system would be used to train residents and expand into other surgical specialties. Today, he predicts new devices will make the surgeon more independent. He envisions a time when surgical technicians have access to the same three-dimensional view as the surgeon.
"I think it’s amazing what they’ve accomplished," says Dr. Schwartz. "We’ve gotten better, we’ve gotten faster, and the length of our hospital stays has hopefully diminished. It’s an incredible piece of equipment, an amazing technological advancement, there’s no question."
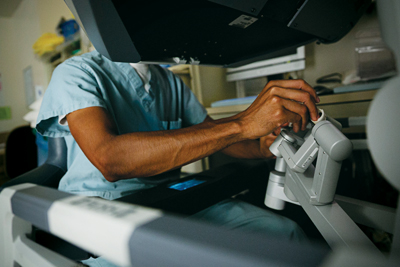
Above Image Caption: Former OB-GYN fellow Tatnai Burnett, MD, and Assaad Semaan, MD, prepare the robot and lock its arms in place before using the console.
